Qliqsoft Secure Hipaa Compliant Healthcare Communication
Electronic health records are an essential component of modern healthcare. they help providers deliver a quality of service that was previously not possible. learn hippa and ehr how hipaa affects your use of ehrs. Nov 10, 2017 ehr and hipaa compliance go hand-in-hand to protect your behavioral health practice from data breaches and government fines. Specific to protecting the information stored in ehrs, the hipaa security rule requires that health care providers set up physical, administrative, and technical safeguards to protect your electronic health information. some safety measures that may be built in to ehr systems include:.
Hipaa Impact On Electronic Health Records Mcguirewoods
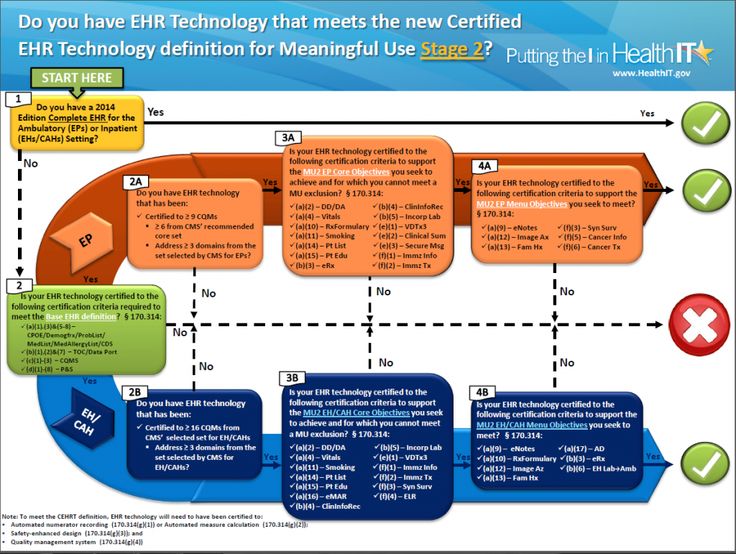
Apr 08, 2013 · the models reflect the regulatory changes of the omnibus rule (2013). in particular, the models highlight the new patient right to access their electronic information held in an electronic health record, if their provider has an ehr in their practice. covered entities may use these models by entering their specific information. See more videos for hipaa and ehr. Ehr implementation is a multi-step process that will impact all staff members. this electronic health record (ehr) implementation guide provides a step by step process for successful planning, implementation, and adoption. learn how to get your healthcare organization on a new ehr software today properly.

Ehr integration care without barriers whether you're trying to protect you patients and staff from infectious diseases like covid-19 or simply trying reach those who cannot make it to an in-person visit, your dedication to quality care does not stop. What is hipaa compliance? providers are now using electronic health records ( ehr) to store patients' electronic protected health information (ephi). Health insurance portability and accountability act of 1996; other short titles: kassebaum–kennedy act, kennedy–kassebaum act: long title: an act to amend the internal revenue code of 1996 to improve portability and continuity of health insurance coverage in the group and individual markets, to combat waste, fraud, and abuse in health insurance and health care delivery, to promote the use. Consent is defined by hippa is for: a. permission to reveal phi for payment of services provided to patients. b. permission to reveal phi for comprehensive treatment of patient. c. permission to reveal phi for normal business operations of the providers facility. d. all the above.
Hipaa Compliance For Emr Ehr Systems Medicalrecords Com
Furthermore, the information the patient inputs into the application is automatically hippa and ehr incorporated in the ehr. a hipaa ba agreement (baa) is a contract between a hipaa-covered entity and a hipaa ba. the contract protects phi in accordance with hipaa guidelines. according to hhs, hipaa ba contracts or other written arrangements should do the.
Health Insurance Portability And Accountability Act

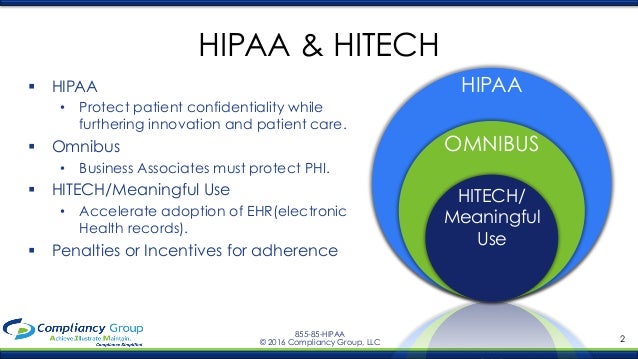
Jan 10, 2021 · tt has been several years since new hipaa regulations have been introduced but that is likely to change very soon. the last update to the hipaa rules was the hipaa omnibus rule changes in 2013, which introduced new requirements mandated by the health information technology for economic and clinical health (hitech) act. Hipaa compliance for emr / ehr systems. the health insurance portability and accountability act which was passed by congress in 1996, specifies who can access or retrieve a patient’s medical records. this law set limits on the use and release of medical records, and established a series of privacy standards for health care providers to follow hipaa compliance. The health insurance portability and accountability act of 1996 (hipaa or the kennedy–kassebaum act) is a united states federal statute enacted by the 104th united states congress and signed into law by president bill clinton on august 21, 1996. it was created primarily to modernize the flow of healthcare information, stipulate how personally identifiable information maintained by the. An ehr may include your medical history, notes, and other information about your also created the hipaa security rule to require specific protections to .
Ehrs can significantly improve healthcare interoperability. but administrators still need to ensure that they are hipaa compliant. Jan 08, 2020 · ehr / emar compatible, paperless environment, secure online interface, gps tracking, hippa compliant direct messaging, automatic high cost alert notifications. pharmacy consulting chart-to-cart audits, survey preparation, flu and vaccination clinics, and other services specifically tailored to maximize the level of care and efficiency of your. Apr 22, hippa and ehr 2021 · nurses with halo, you can reach physicians right when you need them, get just the necessary patient information and alerts on your phone, and coordinate care with the team instantly. no more phone tag! so now you can get back to your real purpose helping patients. learn more > physicians halo enables physicians to consult with on-call colleagues in real-time.
Ehr systems are backed up like most computer systems, so if you are in an area affected by a disaster, like a hurricane, your health information can be retrieved. ehrs can be available in an emergency. if you are in an accident and are unable to explain your health history, a hospital that has a system may be able to talk to your doctor’s system. Under hipaa regulation, ehr data is considered phi because of the amount of sensitive demographic information collected and stored in ehr platforms. ehr providers, therefore, must be hipaa compliant in order to protect clients’ healthcare data from security incidents and government fines. May 4, 2018 a hippa certified ehr does not guarantee compliance. physicians must enact hipaa security standards for using ehr systems and effectively . Had the act not been passed, many healthcare providers would still be using paper records. the act increased the rate of adoption of ehrs from 3. 2% in 2008 to 14. 2% in 2015. by 2017, 86% of office-based physicians had adopted an ehr and 96% of non-federal acute.
Also created the hipaa security rule to require speciic protections to safeguard your electronic health information. a few possible measures that can be built in to ehr systems may include: “access control” tools like passwords and pin numbers, to help limit access to your information to authorized individuals. Sep 19, 2019 · health information technology promises a number of potential benefits for individuals, health care hippa and ehr providers, and the nation’s health care system. Thus, as zoom is not an ehr software or module, our type of technology is not certifiable by these unregulated agencies. saying this, zoom’s hipaa attestation was performed by a third party that reviewed and affirmed that zoom implements.
Privacy, security, and electronic health records hhs. gov.
Privacy and security of health information.
Under hipaa regulation, ehr/emr data is considered phi. therefore, tools that store the records must be hipaa compliant to protect clients’ healthcare data from security incidents, which can cost up to hundreds of thousand dollars. so hipaa and ehr implementation go hand in hand. Aug 21, 2008 hipaa regulations require that covered entities implement administrative, physical and technical safeguards that reasonably and appropriately . Note that hipaa privacy and security rights requires medical records to be retained by a provider for at least six years after either the later of the date of creation or . Nov 14, 2018 hippa and the emr ehr environment. hipaa trouble due to errors in managing electronic health records can be costly. every clinician and emr .